Respiratory Health in Cerebral Palsy
Respiratory Health in Cerebral Palsy
- Section I: Evidence Summary
- Section II: Key Published Evidence
- Section III: Plain Language Summary
- Section IV: Acknowledgments
- Feedback/
Comments
Section I: Evidence Summary Printer Friendly Version
Authors
Authors (AACPDM Respiratory Health in Cerebral Palsy Care Pathway Team): M.S. Cooper (team lead for Care Pathway), A.M. Blackmore, N Gibson, A Chang, L Culloton, J Depiazzi, J Gains, A Jaffe, W Kong, K Langdon, R Marpole, L Moshovis, K Pavleski, A.C. Wilson. Consulting group: G Antolovich, G Baikie, J Chiang, C Fairhurst, AR Harvey, S Louey, P McNamara, M Proesmans, D Reddihough, L Robson, R Ross Russell, N Wimalasundera.
Definitions
Individuals with cerebral palsy (CP) are susceptible to respiratory illnesses such as upper and lower respiratory tract infections, the latter including pneumonia which is commonly due to aspiration. Symptoms of illness may be fever, lethargy, cough, sore throat, runny nose, increased secretions, gurgly breathing or shortness of breath. Oropharyngeal dysphagia (OPD) is the medical term for difficulty swallowing. The motor control issues in CP which cause the physical disability can impact on all stages of swallowing, from closure of lips and formation of a bolus, to the pharynx, larynx and beyond. Oropharyngeal dysphagia or reflux may cause aspiration pneumonia. Poor postural control and subsequent skeletal deformity leads to restrictive lung disease, which is respiratory disease from impaired elasticity of the lungs and mechanics of the chest wall, reducing lung capacity. This contributes to impaired respiratory reserve. A weak cough may cause mucous retention, leading to atelectasis, chronic inflammation, and infection. This may lead to suppurative lung disease, bronchiectasis, and obstructive lung disease.
Issues of respiratory health in CP are interconnected, multifactorial and multisystemic. Treatments may be in the home or require a hospital admission.
Why is Respiratory Health in Cerebral Palsy Important?
- The leading cause of death in children and young people with CP is respiratory illness.
- For adults with CP, death from respiratory illness is 14 times higher than for their peers with no disability.
- For children and young people with CP, respiratory illness is the most common cause of presentation to the emergency department and is the most common cause of prolonged hospital admissions.
- Following an initial respiratory-related admission, the respiratory re-admission rate over the next year is 70%.
- Risk factors can be addressed to minimize aspiration which may help prevent further respiratory illness.
- Treatment of infection should be managed without delay.
- The goal of prevention and treatment is to improve longevity and quality of life for individuals with CP.
Target Population
The risk of respiratory illness should be assessed in all individuals with CP. The strongest predictor for respiratory illness is being classified within Gross Motor Function Classification System (GMFCS) Level V. (This level of GMFCS means any person with CP who uses a wheelchair and is unable to maintain their head or trunk position without adaptive equipment.) Also at high risk is an individual with CP who has had a respiratory admission in the past year, or has been treated with two or more courses of antibiotics for chest infections in the past year. This pathway is for those identified as individuals at high risk of respiratory illness.
Target Clinical Providers
Physicians/Nurses/Therapists caring for individuals with CP.
Assessment
The severity of the respiratory issues for each child will depend on individual factors. However, evidence-based red flags for individuals with CP are: having CP and being classified within GMFCS Level V; having had a respiratory admission in the past year; or having been treated with two or more courses of antibiotics for chest infections in the past year. Important and potentially modifiable risk factors for respiratory illness include: OPD in those < 3 years of age on the Dysphagia Outcome Severity Scale (DOSS) Levels 1-5; or OPD in those > 3 years of age on the Eating and Drinking Ability Classification System (EDACS) Level III-V. (These scores highlight that the presence of any OPD is important.) Other modifiable risk factors include: mealtime respiratory symptoms (gurgly voice, wheezing, coughing, sneezing, choking); frequent respiratory symptoms (daily cough or weekly sounding chesty, phlegmy or wheezy); present or past gastro-esophageal reflux disease (GERD); night-time snoring every night; and uncontrolled epilepsy. Clinicians should identify and manage these risk factors.
A thorough assessment with a respiratory history and physical examination is required. A comprehensive history should include gaining an understanding of concerns, care, comfort and goals. A detailed screen for red flags and potentially modifiable risk factors should be completed. An understanding of swallowing abilities and management of secretions on well and unwell days should be obtained. The physical examination should include the respiratory and heart rate, oxygen saturation level, the pattern of chest wall movement, work of breathing, chest wall shape, palpation and auscultation. Tonsils and turbinates should be visualized. Strength and efficiency of cough should be assessed. Nutritional status should be assessed. Skeletal deformities such as kyphosis and scoliosis should be recorded. Surveillance should be at least annual, with a view to increasing surveillance with any changes in clinical status. Changes in clinical status include: increased respiratory admissions since last review; any respiratory-related concern by family/carers/individual with CP or clinician; evidence of aspiration or change in clinical state affecting ability to manage airway clearance; worsening OPD; difficulties managing secretions or feeds; deterioration in motor skills; or presence of skeletal deformities.
Management
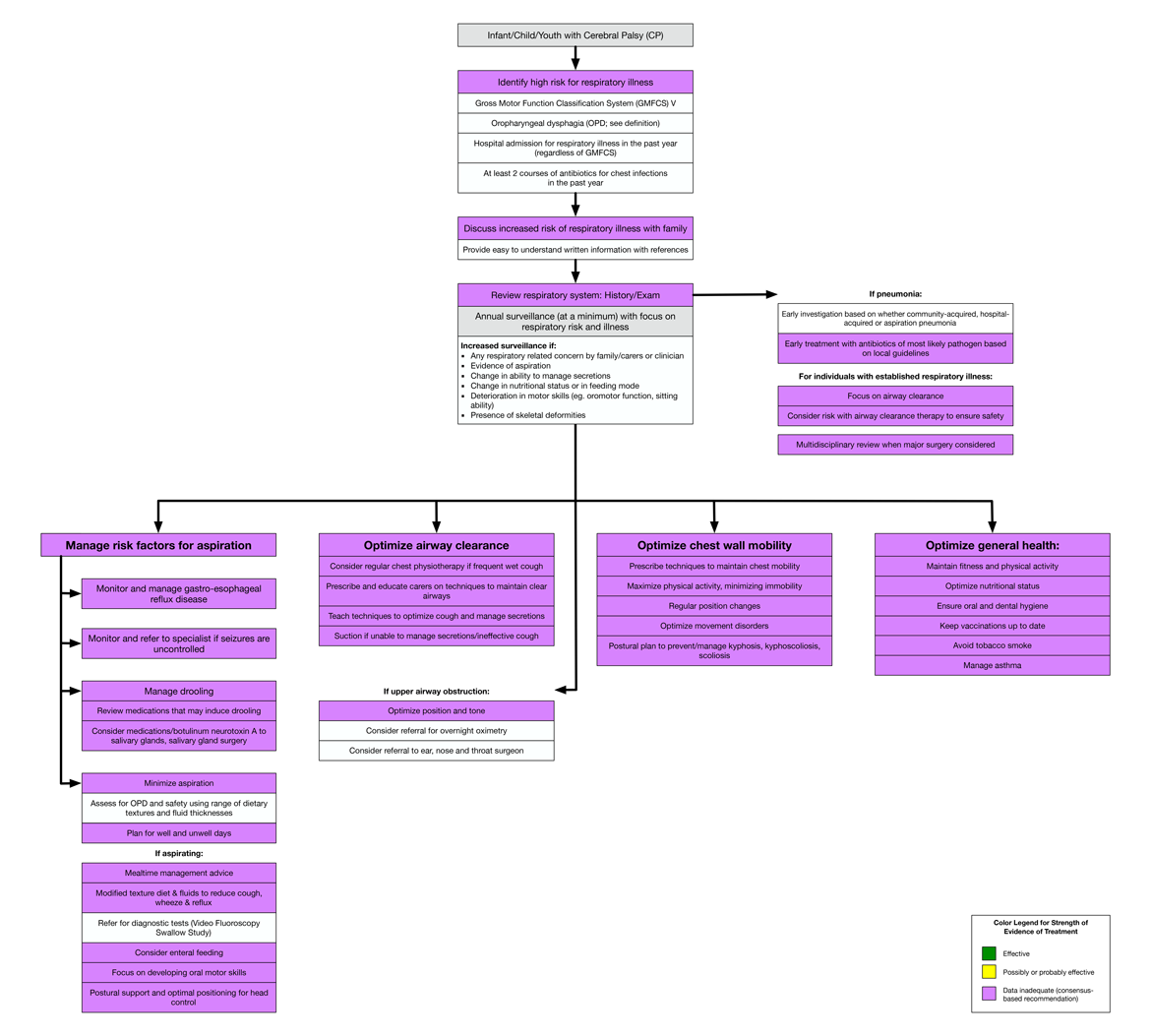
Recognise risk, discuss early and prevent recurrence
- Early discussion about the impact that respiratory health has on morbidity and mortality with parents/carers of children with CP. This is important for those at high risk; namely those with CP classified within GMFCS Level V (or at high-risk of CP) and those with OPD.
- Consider annual surveillance and interdisciplinary assessment and the need for further investigations, referrals and reviews.
- Consider referral to respiratory physician.
Manage risk factors for aspiration
- Optimize gastro-esophageal reflux disease (GERD), seizure control and drooling. (Drooling may be a marker of OPD and management is described in AACPDM Sialorrhea in Cerebral Palsy Care Pathway.)
- Minimize Aspiration
- A clinical assessment of swallowing by a speech pathologist (or occupational therapist).
- Mealtime management prescription includes safe swallow strategies, mealtime positioning and equipment, level of assistance, risk assessment, quality of life needs and informed choice. Mealtime management strategies aim to prevent or reduce cough, wheeze, aspiration and choking.
- A video fluoroscopy swallow study is indicated if ongoing aspiration is suspected, if there are respiratory symptoms or if there is clinical complexity.
- A plan for well and unwell days should be made.
Optimize airway clearance
- Physiotherapist input is recommended for assessment and for prescription, titration and safety of a targeted airway clearance therapy when this is indicated. This includes provision of education to the individual, carer and parents. Suction may be an important adjunct but cease airway clearance therapy if there is risk of aspiration, especially in those with an ineffective cough, respiratory muscle weakness or GERD.
- Assess upper airway. Upper airway obstructive symptoms when awake may be remediable with reduction of tone medications (which may have exacerbated an iatrogenic hypotonia). Reversibility of upper airway obstruction may be assessed by an ear, nose and throat surgeon. Snoring or obstructive sleep apnea may be treated with simpler surgical interventions such as adenoidectomy. Other causes of multilevel obstruction, especially if there are night and day symptoms, require individualized decision making with a multidisciplinary team.
Optimize chest wall mobility
- Physiotherapist and inter-disciplinary input are recommended for assessment, prescription and optimization of chest wall mobility and posture.
Optimize general health
- For example: maintain fitness and physical activities to improve lung health as well as muscle strength, optimize nutritional status and ensure good dental hygiene, keep immunizations up to date, avoid tobacco smoke, and manage concomitant asthma.
Treatment for individuals with pneumonia
- Consider early investigation and treatment of most likely pathogen based on local guidelines.
- Consider airway clearance therapy and suction.
Treatment for individuals with established respiratory illness
- Continue with prevention strategies and regular assessment.
- Continue annual clinical review of the individual focusing on the respiratory system, red flags and modifiable risk factors. Increase surveillance with any changes in clinical status.
- Focus on airway clearance therapy and assess its effectiveness, tolerability and safety.
- For those with recurrent respiratory infections/established respiratory disease, ideally a shared decision model with an interdisciplinary team, primary pediatrician, family/carers and patient is the goal. The team may need to be broadened to include respiratory physicians, surgeons, anesthesiologists, physiatrists or palliative care physicians as needed. Decisions about interventions should take into account the condition and quality of life of the patient. This does not preclude full intensive care or major surgery, if the balance of risk and benefit is agreed to be appropriate.
Flow diagram for evidence-informed Clinical Practice Guideline For Individuals with Cerebral Palsy and High Risk of Respiratory Illness
Respiratory Health Evidence for Interventions
- Interventions for management of respiratory disease in young people with cerebral palsy: A systematic review
- Prevention and management of respiratory disease in young people with cerebral palsy: consensus statement
The purpose of this document is to provide health care professionals with key facts and recommendations for the assessment and treatment of respiratory health in children and youth with cerebral palsy. This summary was produced by M.S. Cooper (team lead for Care Pathway), A.M. Blackmore, N Gibson, A Chang, L Culloton, J Depiazzi, J Gains, A Jaffe, W Kong, K Langdon, R Marpole, L Moshovis, K Pavleski, A.C. Wilson. Consulting group: G Antolovich, G Baikie, J Chiang, C Fairhurst, AR Harvey, S Louey, P McNamara, M Proesmans, D Reddihough, L Robson, R Ross Russell, N Wimalasundera. The summary is based on a systematic review by Blackmore AM, Gibson N, Cooper MS, Langdon K, Moshovis L, Wilson AC. Interventions for management of respiratory disease in young people with cerebral palsy: A systematic review. Child Care Health Dev. 2019 Sep;45(5):754-771. doi: 10.1111/cch.12703. Epub 2019 Jul 30. PMID: 31276598. We did not identify any interventions aimed at preventing respiratory illness in this population. The following algorithm was formulated by consensus-based recommendations: Gibson N, Blackmore AM, Chang AB, Cooper MS, Jaffe A, Kong WR, Langdon K, Moshovis L, Pavleski K, Wilson AC. Prevention and management of respiratory disease in young people with cerebral palsy: consensus statement. Dev Med Child Neurol. 2021 Feb;63(2):172-182. doi: 10.1111/dmcn.14640. Epub 2020 Aug 9. PMID: 32803795; PMCID: PMC7818421.The consensus-based recommendations included recognizing those at risk and managing risks to prevent respiratory illness. However, health care professionals should continue to use their own judgement and take into account additional relevant factors and context. The AACPDM is not liable for any damages, claims, liabilities, or costs arising from the use of these recommendations including loss or damages arising from any claims made by a third party.
Section II: Key Published Evidence
- Blackmore AM, Gibson N, Cooper MS, Langdon K, Moshovis L, Wilson AC. Interventions for management of respiratory disease in young people with cerebral palsy: A systematic review. Child Care Health Dev. 2019 Sep;45(5):754-771. doi: 10.1111/cch.12703. Epub 2019 Jul 30. PMID: 31276598.
- Gibson N, Blackmore AM, Chang AB, Cooper MS, Jaffe A, Kong WR, Langdon K, Moshovis L, Pavleski K, Wilson AC. Prevention and management of respiratory disease in young people with cerebral palsy: consensus statement. Dev Med Child Neurol. 2021 Feb;63(2):172-182. doi: 10.1111/dmcn.14640. Epub 2020 Aug 9. PMID: 32803795; PMCID: PMC7818421.
- Blackmore AM, Bear N, Langdon K, Moshovis L, Gibson N, Wilson AC. Respiratory hospital admissions and emergency department visits in young people with cerebral palsy: 5-year follow-up. Archives of Disease in Childhood. 2019.
- Blackmore, AM, Bear N, Blair E, Langdon K, Moshovis L, Steer K, Wilson AC. Predicting respiratory hospital admissions in young people with cerebral palsy. Arch Dis Child. 2018 Dec;103(12):1119-1124. doi: 10.1136/archdischild-2017-314346. Epub 2018 Mar 19. Erratum in: Arch Dis Child. 2019 Dec;104(12):1215. PMID: 29555725; PMCID: PMC6287554.
- Blackmore AM, Bear N, Blair E, et al. Factors Associated with Respiratory Illness in Children and Young Adults with Cerebral Palsy. J Pediatr. 2016;168:151–7.e1. doi:10.1016/j.jpeds.2015.09.064
- Blair, E., Langdon, K., McIntyre, S. Lawrence, D., Watson, L. Survival and mortality in cerebral palsy: observations to the sixth decade from a data linkage study of a total population register and National Death Index. BMC Neurol 19, 111 (2019).
- Gillam, L. (2106). "The zone of parental discretion: An ethical tool for dealing with disagreement between parents and doctors about medical treatment for a child." Clinical Ethics 11(1): 1-8.
- Meehan, E, Freed, GL, Reid, SM, Williams, K., Sewell, JR, Rawicki, B. Reddihough, D,S. Tertiary paediatric hospital admissions in children and young people with cerebral palsy. Child: Care, Health and Development. 2015;41:6: 928-937
- Meehan, E., Reid, S.M., Williams, K., Freed, G.L., Sewell, J.R., Vidmar, S., Donath, S. and Reddihough, D.S. (2017), Hospital admissions in children with cerebral palsy: a data linkage study. Dev Med Child Neurol, 59: 512-519. doi:10.1111/dmcn.13350
- Ryan, J.M., Peterson, M.D., Ryan, N., Smith, K.J., O'connell, N.E., Liverani, S., Anokye, N., Victor, C. and Allen, E. (2019), Mortality due to cardiovascular disease, respiratory disease, and cancer in adults with cerebral palsy. Dev Med Child Neurol, 61: 924-928. doi:10.1111/dmcn.14176
Section III: Plain Language Summary
Plain Language Summary
‘Evidence-Informed’ Recommendations for the Management of Respiratory Health in Individuals with Cerebral Palsy
Respiratory health in individuals with cerebral palsy (CP) is a major issue which warrants early consideration and discussion. Respiratory illness is the number one cause for unplanned visits to the hospital. Once an individual with CP has one hospital admission for a respiratory infection, over the next 12 months there is a 70% chance of a second admission with a respiratory infection. The hospital admissions are often prolonged and recurrences may have increasing negative effects over time. Respiratory illness due to infection is by far the leading cause of death for individuals with CP.
Long term respiratory issues may present as gurgly breathing and poor management of oral secretions. In CP, the cause of respiratory illness is likely to be due to many related factors. Often the muscles used to maintain good posture and breathe deeply are weaker. This causes difficulty with full opening up of the lungs (especially the lower parts) so they don’t move oxygen effectively. For some, the ability to cough effectively and clear out phlegm is also too weak leading to phlegm being trapped in the lungs, causing inflammation (the body’s reaction to injury) and/or infection. This can lead to slow damage of the lungs which can cause scarring (bronchiectasis). Furthermore, if the individual with CP has an impaired swallow, it may lead to saliva, phlegm, food, fluid and reflux being inhaled into the lungs (aspiration), rather than going down the esophagus (food pipe). This may lead to either a sudden respiratory infection or slow, quiet progressive damage to the lungs. If the individual then develops a major respiratory infection it can be life threatening.
There is evidence to show which individuals with CP are most vulnerable for respiratory illness and aspiration. This includes being classified within Gross Motor Function Classification System Level V (GMFCS V), having difficulty swallowing and having hospital admissions for respiratory illness. People with cerebral palsy GMFCS V have difficulty lifting their head and trunk against gravity and require support for transfers, sitting and mobilization. Individuals with swallowing difficulties are those who need modified textures or tube feeding and those who cough or choke on their saliva. Individuals who are not taking anything by mouth can still have pneumonia from saliva and secretions. An admission to hospital with respiratory illness over the previous year or the need for more than one course of antibiotics in a year also raises concern. Recognition of these important risk factors can enable early management and prevention of illness. Steps may be taken to ensure the swallowing and feeding plan is as safe as possible, reflux disease is treated, night-time snoring is investigated and treated, and uncontrolled epilepsy is managed. We recommend early discussion about respiratory health with your care team, which may include a speech pathologist, occupational therapist, physiotherapist, respiratory therapist, specialized nurse and/or respiratory physician. The team can then set goals focused on prevention of infection and maintenance of respiratory function.
The available evidence is weak with regard to effective measures for prevention and treatment of the risk factors associated with poor respiratory health. This does not mean that these treatments are not worthwhile; rather, it is not possible to make a scientific decision based on evidence alone. It means that current recommendations are based on evidence-informed expert opinion.
In summary, recommendations include early recognition of risk factors for respiratory illness and formulation of plans to limit the negative impact on the respiratory system and to optimize health — these plans often include consideration of an oral eating and drinking plan prescribed by a speech pathologist (or occupational therapist) for feeding, and a physiotherapist prescription of airway clearance therapy to dislodge secretions, move phlegm and encourage deep and effective breathing. General health should be optimized; for example, drooling can be managed with medications, Botulinum toxin injections or surgery; exercising to stay strong and breathe deeply; nutrition honed; regular dental reviews completed; and immunizations prioritized. Respiratory infections should be treated early. Ultimately parents, carers and individuals should be empowered to have a partnership and open discussion with their treating team to optimize respiratory care, limit illness and maximize quality of life.
Helpful Key References:
- Blackmore AM, Gibson N, Cooper MS, Langdon K, Moshovis L, Wilson AC. Interventions for management of respiratory disease in young people with cerebral palsy: A systematic review. Child Care Health Dev. 2019 Sep;45(5):754-771. doi: 10.1111/cch.12703. Epub 2019 Jul 30. PMID: 31276598.
- Gibson N, Blackmore AM, Chang AB, Cooper MS, Jaffe A, Kong WR, Langdon K, Moshovis L, Pavleski K, Wilson AC. Prevention and management of respiratory disease in young people with cerebral palsy: consensus statement. Dev Med Child Neurol. 2020 Aug 9. doi: 10.1111/dmcn.14640. Epub ahead of print. PMID: 32803795.
- Blackmore AM, Bear N, Blair E, et al. Factors Associated with Respiratory Illness in Children and Young Adults with Cerebral Palsy. J Pediatr. 2016;168:151–7.e1. doi:10.1016/j.jpeds.2015.09.064
- Blair, E., Langdon, K., McIntyre, S. Lawrence, D., Watson, L. Survival and mortality in cerebral palsy: observations to the sixth decade from a data linkage study of a total population register and National Death Index. BMC Neurol 19, 111 (2019).
- Gillam, L. (2106). "The zone of parental discretion: An ethical tool for dealing with disagreement between parents and doctors about medical treatment for a child." Clinical Ethics 11(1): 1-8.
- Meehan, E, Freed, GL, Reid, SM, Williams, K., Sewell, JR, Rawicki, B. Reddihough, D,S. Tertiary paediatric hospital admissions in children and young people with cerebral palsy. Child: Care, Health and Development. 2015;41:6: 928-937
- Marpole R, Blackmore AM, Gibson N, Cooper MS, Langdon K, Wilson AC. Evaluation and Management of Respiratory Illness in Children With Cerebral Palsy. Front Pediatr. 2020 Jun 24;8:333. doi: 10.3389/fped.2020.00333. PMID: 32671000; PMCID: PMC7326778.
Practical Tools:
- Gross Motor Function Classification System
https://canchild.ca/system/tenon/assets/attachments/000/002/114/original/GMFCS_English_Illustrations_V2.pdf - Online CP respiratory checklist
https://www.telethonkids.org.au/cpchecklist - Risk factors for respiratory hospital admissions for young people with cerebral palsy
https://onlinelibrary.wiley.com/action/downloadSupplement?doi=10.1111%2Fdmcn.14640&file=dmcn14640-sup-0005-FigS1.pdf - Functional Oral Intake Scale (FOIS)
Crary MA, Carnaby-Mann GD, Groher ME. Initial psychometric assessment of a functional oral intake scale for dysphagia in stroke patients. Arch Phys Med Rehabil 2005;86:1516-1520
https://www.archives-pmr.org/article/S0003-9993(05)00196-6/fulltext - Dysphagia Outcome Severity Scale (DOSS)
O'Neil KH, Purdy M, Falk J, Gallo LJD. The dysphagia outcome and severity scale. 1999;14(3):139- 145.
https://pubmed.ncbi.nlm.nih.gov/10341109/ - Eating and Drinking Ability Classification System (EDACS)
Sellers D, Mandy A, Pennington L, Hankins M, Morris C. Development and reliability of a system to classify the eating and drinking ability of people with cerebral palsy. Dev Med Child Neurol. 2014;56(3):245–251. doi:10.1111/dmcn.12352
https://www.sussexcommunity.nhs.uk/get-involved/research/chailey-research/edacs-request
QUICK REFERENCE:
Recommendations for the prevention and management of respiratory disease in young people with cerebral palsy: Standards of care.
CONSENSUS STATEMENT:
Prevention and management of respiratory disease in you people with cerebral palsy.
Section IV: Acknowledgments
Expert Consensus Team:
|
Name |
Affiliation(s) |
Location |
Specialty Expertise |
|
Monica S. Cooper |
The Royal Children’s Hospital Murdoch Children's Research Institute |
Melbourne, Australia |
Paediatrician Neurodevelopment and Disability |
|
A. Marie Blackmore |
Ability Centre Telethon Kids Institute
|
Perth, Australia |
Research Coordinator Research Associate |
|
Noula Gibson |
Ability Centre Perth Children’s Hospital |
Perth, Australia |
Research Coordinator Physiotherapist |
|
Anne Chang |
Lady Cilento Children's Hospital |
Brisbane, Australia |
Consultant in Paediatric Respiratory Medicine |
|
Lesley Cullotan |
Ability Centre |
Perth, Australia |
Community Coordinator |
|
Julie Depiazzi |
Perth Children's Hospital
|
Perth, Australia |
Physiotherapist |
|
Joan Gains |
Murdoch Children's Research Institute |
Melbourne, Australia |
Community Coordinator |
|
Adam Jaffe |
University of New South Wales Sydney Children’s Hospital, Randwick
|
Sydney, Australia |
Professor of Paediatrics Consultant in Paediatric Respiratory Medicine |
|
WeeRen Kong |
Women’s and Children’s Hospital
|
Adelaide, Australia |
Senior Physiotherapist |
|
Katherine Langdon |
Perth Children's Hospital
|
Perth, Australia |
Paediatric Rehabilitation Physician Paediatric Rehabilitation Medicine |
|
Lisa Moshovis |
Ability Centre |
Perth, Australia |
Clinical Lead – Mealtimes Speech Pathologist |
|
Rachael Marpole |
Perth Children's Hospital
|
Perth, Australia |
Paediatric Respiratory Trainee |
|
Karolina Pavleski |
Ability Centre |
Perth, Australia |
Project Officer |
|
Andrew C. Wilson |
Perth Children's Hospital Princess Margaret Hospital for Children, Telethon Kids Institute School of Paediatrics and Child Health, The University of Western Australia |
Perth, Australia |
Paediatric Respiratory Consultant Clinical Senior Lecturer |
|
Giuliana Antolovich |
The Royal Children’s Hospital Murdoch Children's Research Institute |
Melbourne, Australia |
Paediatrician, Neurodevelopment and Disability |
|
Gordon Baikie |
The Royal Children’s Hospital Murdoch Children's Research Institute |
Melbourne, Australia |
Paediatrician Neurodevelopment and Disability |
|
Jackie Chiang
|
Holland Bloorview Kids Rehabilitation Hospital for Sick Children University of Toronto |
Toronto, Canada |
Paediatric Respirologist |
|
Charlie Fairhurst |
Evelina London Children’s Hospital |
London, United Kingdom |
Consultant in Paediatric Neurodisability
|
|
Adrienne R Harvey |
Murdoch Children's Research Institute The Royal Children's Hospital Melbourne |
Melbourne, Australia |
Team Leader/ Associate Professor of Paediatrics Research Physiotherapist Neurodisability and Rehabilitation |
|
Stefanie Louey |
The Royal Children’s Hospital Murdoch Children's Research Institute |
Melbourne, Australia |
Paediatric Respiratory Trainee Respiratory Medicine |
|
Paul McNamara
|
University of Liverpool, Alder Hey Children's Hospital in Liverpool |
Liverpool, United Kingdom |
Consultant in Paediatric Respiratory Medicine Clinical Senior Lecturer |
|
Marijke |
University Hospital Leuven |
Leuven, Belgium |
Consultant in Pediatric Pulmonology |
|
Dinah S Reddihough |
The Royal Children’s Hospital Murdoch Children's Research Institute |
Melbourne, Australia |
Neurodevelopment and Disability |
|
Lisa Robson |
The Royal Children’s Hospital
|
Melbourne, Australia |
Physiotherapist Neurodevelopment and Disability and Paediatric Intensive Care Unit |
|
Robert |
Addenbrooke's Hospital |
Cambridge, United Kingdom |
Consultant in Paediatric Intensive Care and Respiratory Medicine |
|
Neil |
The Royal Children’s Hospital Murdoch Children's Research Institute |
Melbourne, Australia |
Clinical Director Victorian Paediatric Rehabilitation Service |
|
Maaryasha Werdiger |
Maaryasha Werdiger Physiotherapy |
Melbourne, Australia |
Physiotherapist |
The authors of the care pathway would also like to thank to all participants (clinician, researchers and consumers) for their valuable time and input to construct the consensus-based recommendations.

Feedback/Comments
The American Academy for Cerebral Palsy and Developmental Medicine has developed care pathways to assist the busy clinician. Please submit any advice or constructive feedback to make this pathway more useful.
NOTE: Feedback will be directed to the AACPDM Care Pathway Taskforce to review and consider on a queue 6-month basis.