Cerebral Palsy and Dystonia
Cerebral Palsy and Dystonia
- Section I: Evidence Summary
- Section II: Published Evidence
- Section III: Practical Tools
- Section IV: Acknowledgments
- Feedback/
Comments
Section I: Evidence Summary Printer Friendly Version
Definitions
Dystonia is defined as a “movement disorder characterized by sustained or intermittent muscle contractions causing abnormal, often repetitive movements, postures or both”. Dystonia is commonly seen in cerebral palsy (CP). When muscle contractions are sustained, individuals with CP and dystonia present with stiff postures and hypertonia (sometimes referred to as dystonic hypertonia), which is characterized by resistance to passive stretch of a muscle across a joint, present at low speeds, fluctuates with repeated stretches, and where tactile stimulus or purposeful movement of another body part triggers increased tone or increased involuntary postures. When muscle contractions are intermittent, dystonia typically presents with slow repetitive involuntary movements.
Why is Dystonia in Cerebral Palsy Important?
Dystonia can cause interference in the following ways:
- Dystonia can impede motor function (including speech) through involuntary muscle contractions, limitations in muscle relaxation, and overflow (involuntary activation of unintended muscles during attempted voluntary movement)
- Dystonia can interfere with positioning for sitting and lying
- Dystonic postures and movement can be painful
- Dystonia can interfere with sleep
- Dystonia can result in high energy expenditure and malnutrition
- Dystonic postures/hypertonia can create challenges with caregiving
- Dystonia can impact wellbeing
- Dystonia can be associated with orthopedic deformities
Target Population
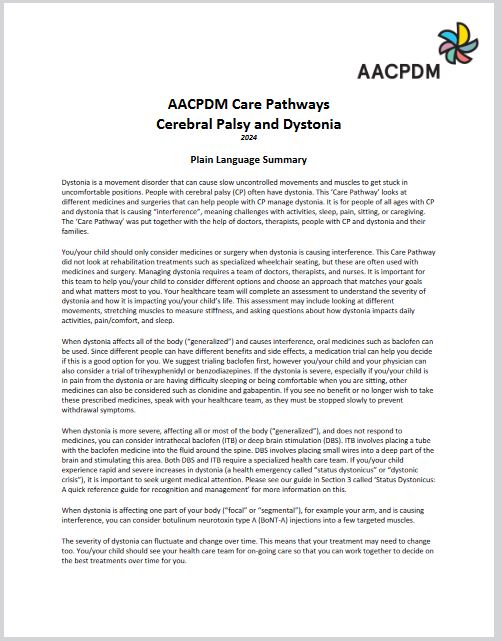
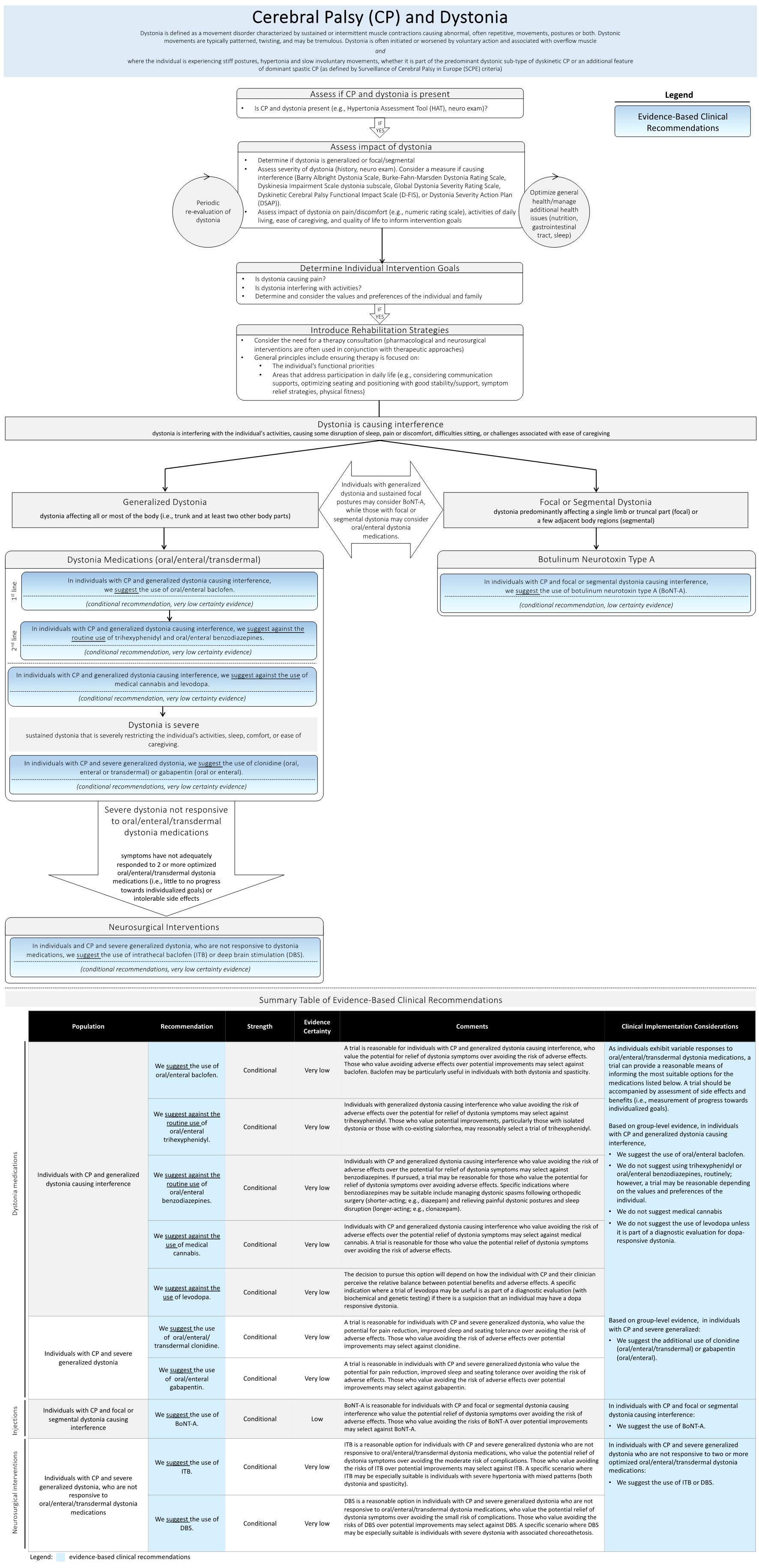
This Care Pathway is focused on pharmacological and neurosurgical interventions intended for individuals of all ages with CP and dystonia who are experiencing stiff dystonic postures, hypertonia, and slow involuntary movements that are causing interference, whether it is part of the predominant dystonic sub-type of dyskinetic CP or an additional feature of dominant spastic CP. Management options directed towards rapid hyperkinetic movements (e.g., tetrabenazine) and recommendations specific to the emergency management of status dystonicus are beyond the scope of this document. The following definitions can be used to help guide interpretation of the more specific population addressed by each recommendation.
Definitions |
|
| Operational definitions pertaining to populations described in recommendations | |
| Dystonia | A movement disorder characterized by “sustained or intermittent muscle contractions causing abnormal, often repetitive, movements, postures or both. Dystonic movements are typically patterned, twisting, and may be tremulous. Dystonia is often initiated or worsened by voluntary action and associated with overflow muscle activation.” |
| Generalized dystonia | Dystonia affecting all or most of the body (i.e., trunk and at least two other body parts) |
| Focal or segmental dystonia | Dystonia predominantly affecting a single limb or truncal part (focal) or a few adjacent body regions (segmental) |
| Dystonia causing interference | Dystonia interfering with the individual’s activities, causing some disruption of sleep, pain or discomfort, difficulties sitting, or challenges associated with ease of caregiving |
| Severe dystonia | Sustained dystonia that is severely restricting the individual’s activities, sleep, comfort, or ease of caregiving. |
| Dystonia not responsive to oral/enteral/transdermal dystonia medications | Individuals whose symptoms have not adequately responded to two or more optimized oral, enteral or transdermal dystonia medications (i.e., little to no meaningful progress towards individualized goals) or who develop intolerable side effects |
| Additional neurologic definitions | |
| Spastic CP | A type of CP with increased tone associated with spasticity (“a velocity-dependent resistance of a muscle to stretch – resistance to externally imposed movement increases with increasing speed of stretch”) |
| Dyskinetic CP | A type of CP with “involuntary, uncontrolled, recurring, and occasionally stereotyped movements. The primitive reflex patterns predominate, and the muscle tone is varying” |
| Chorea | A hyperkinetic involuntary movement consisting of “an ongoing (continuous) random-appearing sequence of one or more discrete involuntary movements or movement fragments”. They frequently appear to be more rapid than dystonia. |
| Athetosis | A “slow, continuous, involuntary writhing movement that prevents maintenance of a stable posture” |
| Myoclonus | A “sequence of repeated, often non-rhythmic, brief shock-like jerks due to sudden involuntary contraction or relaxation of one or more muscles” |
| Status dystonicus | “Status dystonicus is characterized by the development of increasingly frequent or continuous severe episodes of generalized dystonic spasms (contractions) and requires urgent (hospital) management” Status dystonicus is also referred to as dystonic storm or dystonic crisis. |
Target Clinical Providers
Clinicians caring for individuals with CP and dystonia, often led by advanced care providers within multidisciplinary teams.
Assessment
Dystonia is a frequently overlooked element of the neurological presentation of CP. Therefore, it is recommended that a ‘dystonia’ assessment be routinely included in your neurological examination, assessing for fluctuating hypertonia, and using tactile stimulation or voluntary movement to trigger dystonia. More information can be found in Section III of this pathway in the Hypertonia Assessment Tool (HAT) link. On your examination, determine if the dystonia is generalized or focal/segmental and assess the severity. Consider a measure of severity if dystonia is causing interference (e.g., Barry Albright Dystonia Scale, Burke-Fahn-Marsden Dystonia Rating Scale, Dyskinesia Impairment Scale dystonia subscale, Global Dystonia Severity Rating Scale, Dyskinetic Cerebral Palsy Functional Impact Scale, or the Dystonia Severity Action Plan). Assess and monitor the impact of the dystonia on activities/function (e.g., seating tolerance), pain/comfort (including sleep), and ease of caregiving and whether management is required. It is important to jointly identify goals with the individual/family for management.
Management of Dystonia causing Interference
It is important to note that this Dystonia Care Pathway is based on conditional recommendations, as evidence is limited. Shared decision making with the families is therefore essential. The values and preference statements accompanying the recommendations reflect the need for flexibility and factors to consider when selecting a management approach that considers potential benefits and harms and that is aligned with the family’s values and preferences. It is important to first optimize general health and introduce rehabilitation strategies to promote function, comfort, and participation prior to initiating pharmacologic or neurosurgical management.
Rehabilitation Strategies: Evidence specific to rehabilitation strategies is needed before formal recommendations can be developed. Consider the need for a therapy consultation. General principles of therapy include ensuring a focus on the functional priorities of the individual and areas that ultimately address participation in daily life (e.g., optimizing communication, mobility, self-care, symptom relief strategies).
Generalized Dystonia Management: With increasing severity of generalized dystonia, additional interventions may be required beginning with oral medications. For oral medications (also can be given via a g-tube), individuals can experience different benefits and side effects and the introduction of the medication can be guided by response to an individualized trial. Oral baclofen is suggested as a first-line option. Trihexyphenidyl and benzodiazepines should not be used routinely but can be considered as second-line options following a favourable response to a trial. Medical cannabis is not suggested, as side effects appear to outweigh benefits. Levodopa may be used as part of a diagnostic evaluation in cases where a dopa responsive dystonia is suspected. For individuals with severe dystonia, clonidine and gabapentin can be considered, especially for pain, sleep disruption, and seating intolerance. The individual’s response to medication should be monitored, and if there is no response after optimizing the dosage, the medication should be weaned slowly.
In the presence of more severe generalized dystonia that is not responsive to dystonia medications, more aggressive management, such as intrathecal baclofen (ITB) or deep brain stimulation (DBS), is suggested. ITB involves placing a catheter into the fluid around the spinal cord to deliver the baclofen medication. DBS involves placing bilateral electrodes into a deep part of the brain (the globus pallidus internus (GPI) or less commonly the subthalamic nucleus (SN)) and stimulating this area. Both DBS and ITB involve care by a specialized health care team.
Status dystonicus, a health emergency involving rapid and severe increases in dystonia, requires urgent management. While this Care Pathway does not include recommendations specific to the management of status dystonicus, more information with links to helpful resources can be found in our guide in Section 3 (‘Status dystonicus: A quick reference guide for recognition and management’).
Focal or Segmental Dystonia Management: Botulinum neurotoxin type A (BoNT-A) intramuscular injections are suggested for individuals with CP and focal or segmental dystonia causing interference (i.e., dystonia is strongly present in a specific muscle or group or muscles). Consider targeting both the agonist/antagonist muscles around the joint(s) involved with the dystonic posture. Individuals with generalized dystonia and persistent focal postures may also consider BoNT-A, and those with focal or segmental presentations may consider a trial of oral/enteral/transdermal medications.
One of the important features of dystonia is that the severity can fluctuate. This means that the amount of management required can vary and individuals with CP and dystonia should be re-evaluated on a regular basis by the health care team. Standardized outcome measures should be used to monitor the impact of dystonia on individualized goals, activities, pain/comfort (including sleep), caregiving, and quality of life, and whether changes in management are required.
How to interpret the recommendations
All recommendations included in this guideline (see Algorithm) are conditional in strength. Guidance for interpreting recommendations, based on the level of strength, is provided in the table below.
| Guidance for interpretation of strong and conditional recommendations* | ||
| Strong Recommendation | Conditional Recommendation | |
| Wording in the guideline | We recommend… | We suggest… |
| For clinicians | Most individuals should receive the recommended course of action. Adherence to this recommendation according to the guideline could be used as a quality criterion or performance indicator. Formal decision aids are not likely to be needed to help individuals make decisions consistent with their values and preferences. | Recognize that different choices will be appropriate for different individuals, and that you help each individual and family arrive at a management decision consistent with their values and preferences. Decision aids may be useful in helping individuals making decisions consistent with their values and preferences. Clinicians should expect to spend more time with individuals and families when working towards a decision. |
| For individuals with CP and dystonia and their families | Most individuals in this situation would want the recommended course of action and only a small proportion would not | The majority of individuals in this situation would want the suggested source of action, but many would not. |
|
*Adapted from Guyatt, G. H. et al. Going from evidence to recommendations. BMJ 336, 1049-1051, doi:10.1136/bmj.39493.646875.AE (2008). |
||
Algorithm
The purpose of this document is to provide health care professionals with key facts and recommendations for the assessment and treatment of children and youth with dystonia and cerebral palsy. This summary was produced by the AACPDM Dystonia Care Pathway Team (Darcy Fehlings (team lead), Brenda Agnew, Hortensia Gimeno, Adrienne Harvey, Kate Himmelmann, Jean-Pierre Lin, Jonathan W Mink, Elegast Monbaliu, James Rice, Emma Bohn, Yngve Falck-Ytter). The summary is based on a peer-reviewed systematic review. However, health care professionals should continue to use their own judgement and take into account additional relevant factors and context. The AACPDM is not liable for any damages, claims, liabilities, or costs arising from the use of these recommendations including loss or damages arising from any claims made by a third party.
© April 2024, AACPDM Care Pathways
Section II: Published Evidence
 |
Pharmacological and neurosurgical interventions for individuals with cerebral palsy and dystonia: a systematic review update and meta-analysis Authors: Emma Bohn, Katherine Goren, Lauren Switzer, Yngve Falck-Ytter, Darcy Fehlings First published: 27 March 2021 An earlier version of this manuscript was presented at the 2020 American Academy of Cerebral Palsy and Developmental Medicine Conference and was awarded the Gayle G. Arnold Award for best scientific paper. |
 |
Pharmacological and neurosurgical management of cerebral palsy and dystonia: Clinical practice guideline update Authors: Darcy Fehlings, Brenda Agnew, Hortensia Gimeno, Adrienne Harvey, Kate Himmelmann, Jean-Pierre Lin, Jonathan W. Mink, Elegast Monbaliu, James Rice, Emma Bohn, Yngve Falck-Ytter First published: 19 April 2024 |
Section III: Practical Tools
Plain Language Summary
Tools for Classification & Assessment
- SCPE Reference & Training Manual (for identifying CP sub-types)
- Dyskinesia Toolkit
- Hypertonia Assessment Tool (HAT)
Tools for Monitoring
Dystonia
- Barry Albright Dystonia Scale
- Burke-Fahn-Marsden Dystonia Rating Scale
- Dyskinesia Impairment Scale
- Global Dystonia Severity Rating Scale
Individual Goals
- Canadian Occupational Performance Measure
- Goal Attainment Scale
- Performance Quality Rating Scale – Individualized
Pain/Comfort/Sleep
Ease of Caregiving
Quality of Life
- Caregiver Priorities and Child Health Index of Life with Disabilities
- KIDSCREEN-10 (see page 125-127)
Status Dysonicus Recognition & Management
Section IV: Acknowledgments Printer Friendly Version
| Name | Institution | Location | Specialty Expertise |
| Guideline Panel | |||
| Dr. Darcy Fehlings | Holland Bloorview Kids Rehabilitation Hospital; Department of Paediatrics, University of Toronto | Toronto, ON, Canada | Developmental paediatrician |
| Dr. Yngve Falck-Ytter | Veteran Affairs North East Ohio Health Care System Case Western Reserve University | Cleveland, OH, USA | Methodologist |
| Brenda Agnew | N/A | Burlington, ON, Canada | Consumer representative |
| Dr. Hortensia Gimeno | Barts NHS Health and Queen Mary University of London, Wolfson Institute of Population Health, Centre for Preventive Neurology, London, UK | London, UK | Paediatric occupational therapist |
| Dr. Adrienne Harvey | Neurodisability and Rehabilitation, Murdoch Children’s Research Institute | Parkville, Vic, Australia | Paediatric physical therapist |
| Dr. Kate Himmelmann | Department of Pediatrics, Clinical Sciences, Sahlgrenska Academy, University of Gothenburg | Gothenburg, Sweden | Paediatric neurologist |
| Dr. Jean-Pierre Lin | Complex Motor Disorders Service, Evelina London Children’s Hospital Guy’s and St. Thomas’, NHS Foundation Trust; Women’s and Children’s Health Institute, Faculty of Life Sciences & Medicine, King’s Health Partners | London, UK | Paediatric neurologist |
| Dr. Jonathan Mink | Department of Neurology, University of Rochester | Rochester, NY, USA | Paediatric neurologist |
| Dr. Elegast Monbaliu | Neurorehabilitation Technology Lab KU Leuven Campus Brugge, Brugge, Belgium | Leuven, Belgium | Paediatric physical therapist |
| Dr. James Rice | Paediatric Rehabilitation Department, Women's and Children's Hospital | North Adelaide, Australia | Developmental paediatrician |
| Consumer Group | |||
| Brenda Agnew | N/A | Burlington, ON, Canada | Lived experience |
| Lisa Blumberg | N/A | New Haven, CT, USA | Lived experience |
| Kathleen Best | N/A | Ottawa, ON, Canada | Lived experience |
| Shoshana Goldberg | N/A | Toronto, ON, Canada | Lived experience |
| Yemina Goldberg | N/A | Toronto, ON, Canada | Lived experience |
| Lisa Waters | N/A | Atlanta, GA, USA | Lived experience |
| Jaime Winkler | N/A | Saskatoon, SK, Canada | Lived experience |
| Evidence & Administration Group | |||
| Dr. Darcy Fehlings | Holland Bloorview Kids Rehabilitation Hospital; Department of Paediatrics, University of Toronto | Toronto, ON, Canada | Developmental paediatrician |
| Dr. Yngve Falck-Ytter | Veteran Affairs North East Ohio Health Care System Case Western Reserve University | Cleveland, OH, USA | Methodologist |
| Emma Bohn | Holland Bloorview Kids Rehabilitation Hospital; Department of Paediatrics, University of Toronto | Toronto, ON, Canada | Research Assistant |
| Isabelle Caven | Holland Bloorview Kids Rehabilitation Hospital; Department of Paediatrics, University of Toronto | Toronto, ON, Canada | Undergraduate summer research student |
| Lauren Switzer | Holland Bloorview Kids Rehabilitation Hospital; Department of Paediatrics, University of Toronto | Toronto, ON, Canada | Research manager |
| Participants in External Review Process | |||
| Dr. John Andersen | Glenrose Rehabilitation Hospital Department of Pediatrics, University of Alberta | Edmonton, AB, Canada | Neurodevelopmental paediatrician |
| Dr. Giuliana Antolovich | Murdoch Children’s Research Institute Royal Children’s Hospital Melbourne | Parkville, Vic, Australia | Paediatrician |
| Dr. Bhooma Aravamuthan | Washington University School of Medicine | St. Louis, MO, USA | Paediatric movement disorders neurologist |
| Dr. Lynn Bar-On | Ghent University, Department of Rehabilitation Sciences | Ghent, Belgium | Physiotherapist |
| Dr. Mohan Belthur | Department of Child Health & Orthopedics, University of Arizona College of Medicine – Phoenix; Department of Orthopedics, Phoenix Children’s Hospital | Phoenix, AZ, USA | Paediatric orthopaedic surgeon |
| Dr. Alfred Peter Born | Rigshospitalet | Copenhagen, Denmark | Paediatric neurologist |
| Dr. Roslyn Boyd | Child Health Research Centre, Queensland Cerebral Palsy and Rehabilitation Research Centre, The University of Queensland | Brisbane, Qld, Australia | Physiotherapist |
| Erin Brandon | Holland Bloorview Kids Rehabilitation Hospital | Toronto, ON, Canada | Paediatric nurse practitioner |
| Dr. Annemieke Buizer | Amsterdam UMC, Vrije Universiteit Amsterdam, Department of Rehailitation Medicine, Amsterdam Movement Sciences Emma Children’s Hospital, Amsterdam UMC | Amsterdam, Netherlands | Paediatric physiatrist |
| Dr. Leon Dure | University of Alabama at Birmingham | Birmingham, AL, USA | Pediatric neurologist |
| Dr. Hernan Gonorazky | The Hospital for Sick Children University of Toronto | Toronto, ON, Canada | Paediatric neurologist |
| Dr. Mark Gormley | Department of Physical Medicine and Rehabilitation, Gillette Children’s Specialty Healthcare | St. Paul, MN, USA | Paediatric physiatrist |
| Dr. Jan-Willem Gorter | CanChild Centre for Childhood Disability Research, Department of Pediatrics, McMaster University; McMaster Children’s Hospital | Hamilton, ON, Canada | Paediatric physiatrist |
| Dr. Anne Kawamura | Holland Bloorview Kids Rehabilitation Hospital | Toronto, ON, Canada | Developmental paediatrician |
| Dr. Michael Kruer | Pediatric Movement Disorders Program, Barrow Neurological Institute, Phoenix Children’s Hospital | Phoenix, AZ, USA | Paediatric neurologist |
| Dr. Anne Koy | University Hospital Cologne Department of Pediatrics, University of Cologne | Cologne, Germany | Paediatric neurologist |
| Jennifer Lewis | Kids Rehab, The Children’s Hospital at Westmead | Sydney, NSW, Australia | Physiotherapist |
| Dr. Claire Lundy | Royal Belfast Hospital for Sick Children | Belfast, UK | Consultant in paediatric neurology and neurodisability |
| Dr. Amber Makino | Holland Bloorview Kids Rehabilitation Hospital | Toronto, ON, Canada | Developmental paediatrician |
| Dr. Anna McCormick | Children’s Hospital of Eastern Ontario Department of Pediatrics, University of Ottawa | Ottawa, ON, Canada | Paediatric physiatrist |
| Dr. Scott McLeod | Department of Pediatrics, University of Calgary | Calgary, AB, Canada | Developmental paediatrician |
| Dr. Ronit Mesterman | Department of Pediatrics, McMaster University | Hamilton, ON, Canada | Paediatric neurologist & developmental paediatrician |
| Dr. Santosh Mordekar | Sheffield Children’s Hospital | Sheffield, UK | Paediatric neurologist |
| Dr. Roser Pons | Aghia Sofia Children’s Hospital; National and Kapodistrian University of Athens | Athens, Greece | Paediatric neurologist |
| Dr. Simon Schless | ALYN Paediatric and Adolescent Rehabilitation Hospital | Jerusalem, Israel | Physiotherapist |
| Dr. Jordan Sheriko | Department of Pediatrics, Dalhousie University | Halifax, NS, Canada | Paediatric physiatrist |
| Nadine Smith | Departments of Physiotherapy and Kids Rehab WA, Perth Children’s Hospital | Nedlands, WA, Australia | Physiotherapist |
| Dr. Kirsty Stewart | The Children’s Hospital at Westmead | Sydney, NSW Australia | Occupational therapist |
| Dr. Ellen Wood | Department of Pediatrics, Dalhousie University | Halifax, NS, Canada | Paediatric neurologist |

Feedback/Comments
The American Academy for Cerebral Palsy and Developmental Medicine has developed care pathways to assist the busy clinician. Please submit any advice or constructive feedback to make this pathway more useful.
NOTE: Feedback will be directed to the AACPDM Care Pathway Taskforce to review and consider on a queue 6-month basis.